- Suspected mpox cases across the continent have surged past 17,000—a sharp increase from 7,146 cases in 2022 and 14,957 cases in 2023.
- The disease has rapidly spread from the epicentre, DRC to at least 13 African countries, including nations previously unaffected such as Burundi, Kenya, Rwanda, and Uganda.
- Already, Africa CDC has entered into an alliance to provide over 215,000 doses of the MVA-BN® vaccine—the only Mpox vaccine approved by the FDA and EMA.
The Africa Centres for Disease Control and Prevention (Africa CDC) has declared the ongoing Mpox outbreak as a Public Health Emergency of Continental Security (PHECS).
This declaration is the first of its kind since the agency’s establishment in 2017, marking a critical moment in Africa’s public health scene even as authorities step up measures to tackle an outbreak of this deadly disease.
Under the authority granted by Article 3, Paragraph F of the Africa CDC Statutes, this declaration empowers the organization to take the lead in coordinating and managing health emergency responses across the continent.
The statute mandates Africa CDC to not only respond to health emergencies but also to strengthen health systems, address communicable and non-communicable diseases, and tackle environmental health and Neglected Tropical Diseases.
PHECS declaration will put in place initiatives and measures for the mobilization of resources, unlocking essential funding, and enhancing the continent’s capacity to respond to the Mpox outbreak.
Dr. Jean Kaseya, Director General of Africa CDC, emphasized the urgency of this declaration, stating, “Today, we declare this PHECS to mobilize our institutions, our collective will, and our resources to act—swiftly and decisively. This empowers us to forge new partnerships, strengthen our health systems, educate our communities, and deliver life-saving interventions where they are needed most. There is no need for travel restrictions at this time.”

The alarming spread of Mpox in Africa
The Mpox outbreak has rapidly spread across at least 13 African countries, including nations previously unaffected by the virus, such as Burundi, Kenya, Rwanda, and Uganda.
In 2024 alone, these countries have confirmed a total of 2,863 cases and 517 deaths, with the majority of cases reported in the Democratic Republic of the Congo (DRC).
The situation is even more concerning when considering the suspected cases across the continent, which have surged past 17,000—a significant increase from 7,146 cases in 2022 and 14,957 cases in 2023.
These numbers underscore the urgent need for coordinated action, especially given the weaknesses in surveillance, laboratory testing, and contact tracing.
Dr. Kaseya cited the gravity of the situation, stating, “This is not just another challenge; it’s a crisis that demands our collective action. Article 3, Paragraph F of the Africa CDC Statutes mandates us to lead and coordinate the response when there is a declaration of a public health emergency of international concern.”
Global support: A call to action
The global response to the Mpox outbreak in Africa has been notably lacking. From May 2022 to July 2023, Mpox was declared a Public Health Emergency of International Concern (PHEIC) by the World Health Organization (WHO).
However, despite the urgent need, Africa did not receive the necessary support during this period. As global cases began to decline, the escalating numbers in Africa were largely overlooked.
Dr. Kaseya called for a change in approach, urging international partners to act differently this time around. “We urge our international partners to seize this moment to act differently and collaborate closely with Africa CDC to provide the necessary support to our Member States,” he stated.
The Director General also appealed directly to global partners, emphasizing the need for a united response to the crisis. “We call on you to stand with us in this critical hour. Africa has long been on the frontlines in the fight against infectious diseases, often with limited resources. The battle against Mpox demands a global response. We need your support, expertise, and solidarity. The world cannot afford to turn a blind eye to this crisis.”
Africa CDC’s emergency declaration follows consultations, including a unanimous decision by the Africa CDC Emergency Consultative Group (ECG), chaired by Professor Salim Abdool Karim, head of CAPRISA, an AIDS research program based in Durban, South Africa.
Read also: Gene-editing technique promises to erase HIV from infected cells
A growing threat: Mpox and HIV
Professor Karim highlighted the increasing severity of the Mpox outbreak, noting that limited surveillance and evidence suggest the situation could be more dire than currently understood.
“The number of cases has significantly increased compared to 2022 when WHO declared Mpox a public health emergency. It’s clear that we’re facing a different scenario with far more cases, resulting in a higher burden of illness,” he said.
A particular area of concern is the rising fatalities linked to Mpox, especially in conjunction with HIV. “Our concern is that we may be seeing more fatalities in Africa due to the association with HIV,” Professor Karim noted. This alarming trend underscores the need for targeted interventions to address the unique challenges posed by the intersection of Mpox and HIV, particularly in regions with high HIV prevalence.
Cross-border transmission and the urgency for vaccines
The cross-border transmission of Mpox to previously unaffected countries has added another layer of complexity to the outbreak. This spread has prompted the ECG to recommend the strategic distribution of the limited vaccines available.
The lack of diagnostic capabilities in many affected countries has also been identified as a critical issue that requires immediate attention. The ECG has encouraged the development of comprehensive response plans, promising to provide input and support as needed.
In response to the outbreak, Africa CDC has established a 25-member Incident Management Team based at the epicenter of the Mpox epidemic. This team is tasked with supporting affected and at-risk countries, ensuring that the response is swift and effective.
Strengthening Africa’s Mpox response
To bolster the continent’s response to the Mpox outbreak, Africa CDC has entered into a partnership with the European Commission’s Health Emergency Preparedness and Response Authority (HERA) and Bavarian Nordic.
This collaboration will provide over 215,000 doses of the MVA-BN® vaccine—the only Mpox vaccine approved by the FDA and EMA. Africa CDC will oversee the equitable distribution of these vaccines, prioritizing the needs of affected Member States and ensuring that the most vulnerable populations receive the necessary protection.
Mpox outbreak: Symptoms, prevention, and treatment
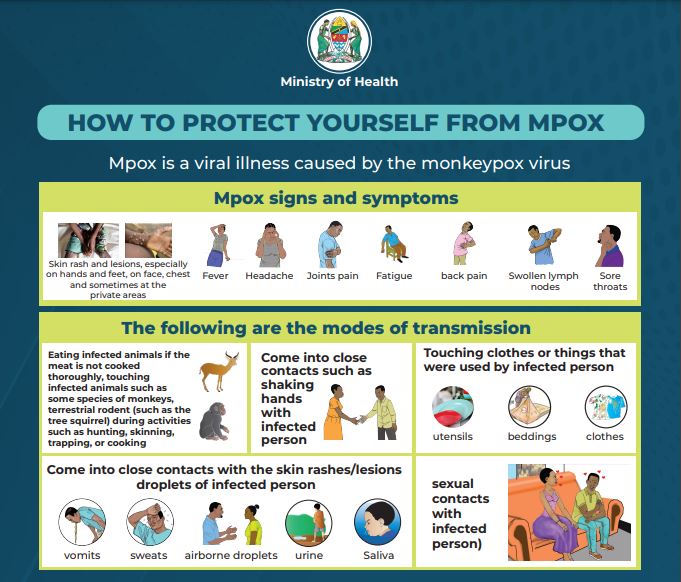
Mpox is a viral illness caused by the monkeypox virus, with two distinct clades: Clade I and Clade II. The virus is primarily transmitted to humans through physical contact with an infectious person, contaminated materials, or infected animals.
Common symptoms of Mpox include a skin rash or mucosal lesions that can last two to four weeks, fever, headache, muscle aches, back pain, low energy, and swollen lymph nodes.
Preventing the spread of Mpox requires vigilant public health measures, including effective surveillance, prompt diagnosis, and targeted vaccination campaigns.
To help tackle the menace, infected individuals should be isolated to prevent further transmission, and communities must be educated about the symptoms and transmission routes of Mpox.
The declaration of Mpox as a Public Health Emergency of Continental Security by Africa CDC marks a critical moment in the continent’s ongoing battle against infectious diseases. This declaration is not just a call to action for Africa but a plea to the global community to recognize the severity of the situation and respond with the necessary support.
As Dr. Kaseya noted, “This is a crisis that demands our collective action.” The success of Africa’s response to Mpox will depend on the swift mobilization of resources, the strengthening of health systems, and the unwavering support of international partners.
Only through a united and coordinated effort can the continent overcome this challenge and protect the health and well-being of its people.











